Every operation involves some risk. Here are the main risks associated with thyroid surgery:
Hoarse Voice: The recurrent laryngeal nerves are important nerves that control the vocal cords and your voice. If the nerve is irritated during the operation, it stops sending signals to the vocal cords, which gives patients a hoarse voice. This can also cause difficulty swallowing thin liquids like water, since the vocal cord also help block liquids from splashing into the airway. There is a 5-7% risk of temporary hoarseness that gets better on its own as the nerve has time to recover. There is a 0.5% risk of permanent nerve injury. If that occurs, the voice can still be brought back to normal with additional procedures. Nerve monitoring can be used to preict the function of the nerves but does not prevent injury.
Change in Projection / Singing Voice: The external branch of the superior laryngeal nerve is another nerve that lives just above the thyroid. This nerve controls a muscle that helps you project your voice and reach a high pitch when singing. Risk of injury is low, but can result in change in singing voice and ability to yell. The most common voice change is deepening of the voice from scarring on the muscles and nerves on the outside of the voice box.
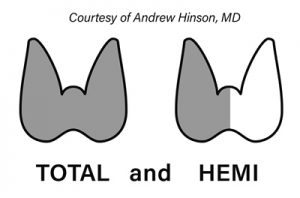
Low Calcium / Hypoparathyroidism: The parathyroid glands are four tiny glands that live next to the thyroid and control our body’s calcium levels. When patients undergo total thyroidectomy, there is a 1-3% chance that all four glands can be damaged or accidentally removed, there is also the risk that 1-2 of the parathyroid glands are affected but not all. If that happens, patients will not have enough parathyroid hormone, causing them to have low blood calcium. The main symptom of low calcium is typically numbness and tingling in the digits and around the lips. In severe cases, it can cause muscle cramps. When patients undergo thyroid lobectomy, there is no risk of low calcium. Low calcium is treated with oral calcium and vitamin D.
Wound Infection: Less than 1% of patients will experience a wound infection. Since the neck is a clean area this happens very infrequently. Infections are typically treated with antibiotics, but may need surgical drainage in severe cases.
Neck Hematoma: Rarely, bleeding after surgery can lead to a build-up of blood in the neck called a hematoma. This can lead to neck swelling and bruising. When severe, this can cause difficulty breathing and require emergency surgery. Bleeding usually occurs in the first 2 hours after surgery, but patients will need to avoid heavy lifting for 2 weeks.